Laser therapy in the treatment of persistent idiopathic orofacial pain and traumatic trigeminal neuropathy
Keywords:laser, treatment, medical, fiber, Time:17-11-2015There are only few studies regarding the use of LLLT for nerve recovery in humans and rats. It seems that LLLT act analgesically since they improve endorphin release and therefore inhibit nociceptive signals and control pain mediators [2]. Low level lasers can also act analgesically by inhibiting pain signals which partially leads to the transient varicosities along the neurons which decrease impulse transmission. Cells are acidic in a lowered redox state, but after laser irradiation they become alkaline and afterwards they can act in an optimal way. It is well known that LLLT stimulate lymphocytes, activate mast cells, and increase production of adenosine triphosphate in the mitochondria and proliferation of various cell types therefore acting as antiinflammatory [2]. Furthermore, LLLT stimulate microcirculation which results in the change of capillary hydrostatic pressure which in turn results in edema absorption and elimination of intermediary metabolites [2]. Rochkind et al., [3] reported that in patients with long-term peripheral nerve injury noninvasive which leads to significant functional recovery. GigoBenato et al., [4] reported that 660 nm LLLT with low (10 J/cm2) or moderate (60 J/cm2) energy densities is able to accelerate neuromuscular recovery after nerve crush injury in rats. Peric [5] reported that LLLT (30 treatments during a period of 12 weeks) in patients with diabetic polyneuropathy (control group was given only vitamin therapy) showed decrease in spatial perception threshold and increase in motor medianus conduction. Ohtsuka et al., [6] treated patient with postherpetic neuralgia which manifested as burning pain in the right forehead with LLLT which resulted in the increased blood flow and relieve in neuralgia. Persistent idiopathic orofacial pain (PIFP) is characterized by poorly localized pain and perceived as arising from muscles of the face and jaw. Symptoms wax and wane in intensity over days and weeks [7]. Traumatic trigeminal neuropathy is usually induced by oral surgical operations, particularly the removal of the impacted lower third molars, being more frequent in females. It can manifest itself with various degrees of sensory loss [8].
Methods
Twenty one patients, 10 with persistent idiopathic facial pain (PIFP) and 11 with traumatic trigeminal neuropathy (TTN) were involved in this study. Diagnosis of PIFP was carried out according to criteria established the Headache Classification Subcommittee of the International Headache Society [9]: (1) Facial pain present daily for at least 1 month and persisting for all or most of the day. (2) The pain is deep and poorly localized of moderate or severe intensity, but not unbearable. (3) The pain is confined at onset to a limited area on one side of the head. (4) The pain is without paroxysms, precipitation from trigger areas, autonomic symptoms, sensory loss, and other physical signs; but dysaesthesia may occur. Diagnosis of TTN was made upon these criteria: (1) sensory defect (paraesthesia) in the region innervated by maxillary or mandibular nerve following surgical procedure and (2) minimal duration of 3 months. Three experienced dentists who are also academic staff from the Department of Oral medicine, University of Zagreb in Croatia diagnosed the painful conditions. The exclusion criteria were other orofacial pain conditions due to odontogenic causes, vascular conditions (migraine, etc) and inability of patient to understand the text of the informed consent. None of the patients had systemic diseases nor took meds that might affect their pain. The study was approved by the Ethical Committee of the University of Zagreb in Croatia and from every patient informed consent according to Helsinki II declaration was obtained.
Laser procedure
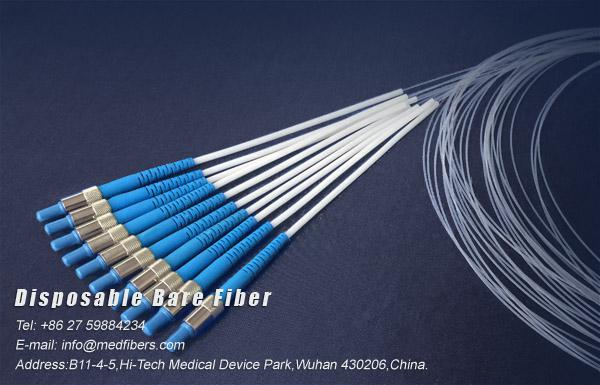
Laser Fibers therapy was performed with a galium-aluminumarsenide (GaAlAs) laser (BTL-5000,www.medfibers.com) with wavelength of 830 nm. Each session was performed on every working day and lasted for 3 min (total number of 10 days). Break was during the weekend. There were two irradiation cycles during one session, according to the manufacterer’s recommendations for the treatment of trigeminal neuralgia. First cycle was A and consisted of 12 J/cm2, duty factor 100%, cont.area 1.00 cm2, max power 100 mW, duration 2 minutes and second cycle was 6 J/cm2, duty factor 80%, 10 Hz, area 1 cm2, max power 100 mW, duration 1 min and 15 sec. We did not use placebo as we thaught that patients would suffer even more as they were not given any therapy and were already in much pain. In the case of medical fiber optics was applied on the skin at the most painful surface area (1 cm2). In the case of TTN laser application area was on the lingual side ofthe mandible at the extraction site where the surgical injury occurred.
Evaluation and statistical analysis
Primary endpoint was patients’ report on the relief of symptoms (0=no improvement,1=partial improvement,2=complete improvement). Statistical analysis was performed by use of descriptive statistics (mean and standard deviation). Differences between the tested groups were assesed by chi-square test. Values lower than 0.05 were considered significant.
Results
Clinical characteristics of the patients are presented in Table 1. No significant differences in terms of age and gender were found between the two patient groups (PIFP vs. TTN, p=0.077; p=0.645). Total resolution of symptoms was achieved in 70% of patients with PIFP and 36.4% of patients with TTN. Partial resolution of symptoms was achieved in 20% of patients with PIFP and 18.2% of patients with TTN. Treatment showed no improvement in 10% of patients with PIFP and 45.4% of patients with TTN. No significant differences in outcome were found between the two groups (p=0.302).
Discussion and conclusion
Most of the patients had 12 applications (twice a week) with an average dose of 1.8 J/ cm2. Most treatment consisted of a series of 12 applications (twice a week) and in 15 cases a second series was applied. Patients were treated with an average dose of 1.8 J/cm2. One hundred fifty four out of 241 patients were asymptomatic at the end of the treatment, 50 improved considerably, and 37 were symptomatic. The results confirmed that LLLT is an effective tool and is beneficial for the treatment of many disorders in the maxillofacial region. Miloro and Repasky [12] demonstrated that neurosensory recovery after bilateral saggital split osteotomy can be significantly improved both in terms of time course and magnitude of return of function with the adjunctive use of LLLT. The authors used LLLT (4×6 J per treatment, along the distribution of the inferior alveolar nerve before surgery, 6 and 24 h after and on the 2nd, 3rd, 4th and 7th day). Ozen et al., [13] treated four female patients after third molar surgery who had paraesthesia with LLLT (GaAlAs laser, the irradiance used was 6 J per treatment site, applying 5 mW in continuous mode wave for 90 s in total of 20 treatments performed every second day) and concluded that LLLT reduces long-standing sensory nerve impairment following third molar surgery. Saber et al., [14] concluded that there was a significant difference in pain level between laser and placebo group after third molar surgery, however there was no difference in pain duration between the two tested groups. On the other hand, Lopez-Ramirez et al., [15] reported that LLLT (810 nm, output power 0.5 W and 5 J/cm2 energy density) did not show beneficial effects in reducing pain, swelling and trismus after extraction of the impacted molars. Eckerdal and Bastian [16] treated patients with laser (830 nm, 30 mW) for five weeks. The results demonstrated that out of 16 patients, ten were painfree, two had decreased pain levels while in four there was no change. Moore et al., [17] also evaluated the use of Ga-Al-As diode laser (830 nm, 60mW) in patients with postherpetic neuralgia and demonstrated significant reduction in the pain intensity in their patients. More recent studies such as one of Yang and Huang [18] studied LLLT in 16 patients with persistent idiopathic orofacial pain (PIFP) and average pain reduction of 43.47% (ranging from 9.3% to 91.8%) was achieved which is lower percentage in comparison to our sample (70%). However, hteir patients received LLLT between one to ten times, whereas all our patients received the same LLLT regimen (ten times altogether). The same authors concluded [18] that LLLT may be an effective treatment for PIFP. On the other hand, Tengrungsun et al., [19] concluded on the literature systematic review that there is only limited evidence suggesting that LLLT is more effective than placebo, sham laser and other active treatment in the treatment of orofacial pain.
Related Articles
- Indications and limitations of Er:YAG laser applications in dentistry
- LOW LEVEL LASER THERAPY
- Laser Fibers Application in Periodontics
- Study on the Influence of Semiconductor Laser Irradiated Time towards Dental Pulp and Dentin
- Global Industry Analysis on Medical Laser Technology Market, 2015 to 2021
- APPLICATION OF Nd–YAG LASER TREATMENT FOR ORAL LEUKOPLAKIA
- Medfibers:Diode Lasers for Periodontal Treatment
- Interventional laser surgery for oral potentially malignant disorders: a longitudinal patient cohort study
- Topical Gel Application and Low Level Laser Therapy on Related Soft Tissue Traumatic Aphthous Ulcers
- The TwinLight™ Concept in Dentistry Reviews
